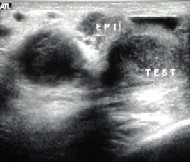
The following images show examples of normal and abnormal ultrasounds. Click on any image for an enlargment.
After an orchiectomy, in which the testicle and its attached plumbing is removed, the diseased tissue is sent to a pathologist for examination. The pathologist will determine whether the tissue is a malignant tumor, and if so, whether it is a seminoma (tumors composed of sperm-producing cells) or non-seminoma. The pathologist will also look for neoplasm (cancerous tumors) in the epididymis, seminal ducts, lymph vessels and blood vessels to gain an indication of whether the cancer has spread beyond the testicles.
Blood and urine tests will be used to check for signs of infection, and to measure tumor serum markers, such as beta-HCG, AFP, and LDH.
A CT scan of the pelvis, abdomen and chest, and a chest x-ray will be used to determine whether the cancer has spread beyond the testicles. This is often referred to as the staging of the cancer.
Causes | Checklist | Costs | Cancer Jokes | Cancer Scholarships | Sites